RELATED Live.
- About us
- KIMA Members
-
KIMA Doctors
- All
- Anesthesiology
- artificial joint center
- Breast and Endocrine Surgery
- Breast cancer and thyroid cancer center
- Breast Surgery
- Cardiology
- Cardiothoracic Surgery
- Cerebrovascular Center
- Colorectal Surgery
- dental and maxillofacial surgery
- Dermatology
- Endocrinology
- Gastroenterology
- General Surgery
- Genito-Urology
- Hematology
- Hemato-oncology
- Infection Center
- Internal Medicine
- International Healthcare Center
- Korean Medicine
- liver center/Pancreas and billiary tract center
- Liver Transplantation
- Neurology
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopedic
- Otorhinolaryngology
- Pediatric & Juvenile
- Pediatric Allergy and Respiratory Diseases
- Pediatric Gastroenterology
- Pediatric Neurology
- Pediatrics
- Physical Medicine & Rehabilitation
- Plastic & Reconstructive Surgery
- plastic surgery
- Pulmonology
- Radiation oncology
- Rheumatology
- Thyroid & Endocrine Surgery
- Urology
- Vascular Surgery
- KIMA News
- KIMA Live
- Community
KIMA NEWS
Identification of how cancer stem cells survive in the presence of anticancer drugs
Simultaneous administration of an anticancer agent and a lead compound developed by the research team to inhibit cancer cell growth 10 times more effectively
A new drug candidate showing therapeutic effects against cancer that has recurred or metastasized because it is unresponsive to anticancer drugs has been developed.
A research team led by Dr. Cheong Jae-ho and Dr. Park Ki-cheong from the School of Surgery at Yonsei University College of Medicine announced on February 13 that they had identified how cancer stem cells gain resistance against existing anti-cancer drug treatments and found a lead compound to overcome this issue.
The results of this study were published in the latest issue of the international medical journal BMC Medicine (IF11.8).
Stem cells in our body continuously enable growth and regeneration. About 1 to 2% of all cancers have what are called “cancer stem cells” that give them the ability to continually renew themselves. That is, they are able to regenerate themselves and differentiate into other cells, which increases the chance of recurrence and metastasis.
In the case of normal cancer cells, they die in the presence of anticancer drugs, which deteriorate the tumor microenvironment. This is because when cancer cells are under continuous endoplasmic reticulum stress from anticancer drugs, calcium ions secreted by the protein IP3R start to accumulate in the mitochondria of the cells.
However, in some patients, cancer stem cells are activated and exhibit particularly strong resistance to anticancer drugs. When the resistance is extremely strong and the cancer is impossible to treat with conventional chemotherapy, it is classified as refractory cancer.
The research team first confirmed the principle behind the survival of anticancer drug-resistant cancer cells. An analysis of cancer cells collected from patients whose cancer had relapsed or metastasized while taking anticancer drugs showed that there were anticancer drug-resistant cancer cells with cancer stem cells. It was also found that when the protein PMCA increases significantly in cancer stem cells, the calcium ion concentration drops, thereby allowing cancer cells to survive.
Accordingly, the research team developed a lead compound (Candidate 13) to inhibit PMCA, a protein that boosts anticancer drug resistance. Subsequently, the effectiveness of treatment was examined by conducting an animal experiment in which a standard anticancer drug and the lead substance were administered concurrently.
First, cancer cells from patients who had experienced relapse or metastasis due to resistance to the standard anti-cancer drugs, oxaliplatin and sorafenib, were grafted onto animal models, and then each drug was administered alone to check the changes in tumor size over time.
When only oxaliplatin was administered, the tumor, which was originally 200 mm3 in size on average, continued to grow to 354.44 mm3 in 20 days, 1,593.2 mm3 in 30 days, and 2,756.36 mm3 in 40 days. This was similar to the results obtained from the group that was administered sorafenib, whose tumor size grew to 365.26 mm3 in 20 days, 1,116.26 mm3 in 30 days, and 2,998.77 mm3 in 40 days.
Then the size of the tumor was measured after administering oxaliplatin, sorafenib, and the lead compound in combination, and it showed that the tumor growth rate slowed.
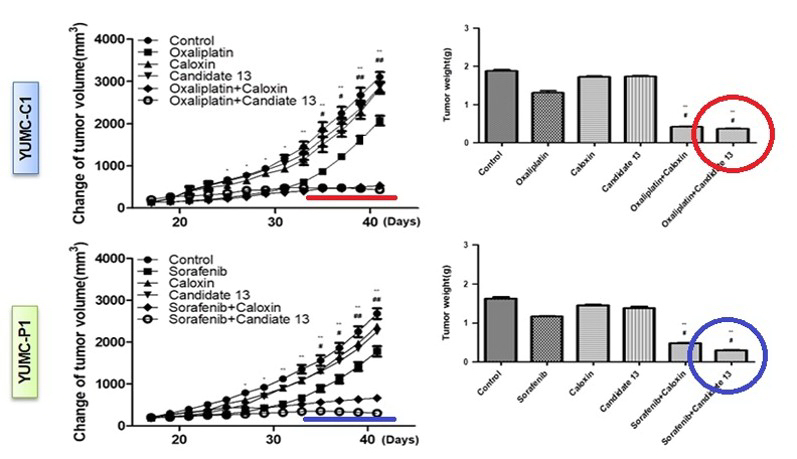
When oxaliplatin and the lead compound were concomitantly administered, the tumor that was initially 200 mm3 in size grew to 254.32 mm3 in 20 days, 288.41 mm3 in 30 days, and 283.44 mm3 in 40 days.
Similarly, when sorafenib and the lead compound were administered in combination, the tumor measuring 200 mm3 at the beginning grew to 274.33 mm3 in 20 days, 303.14 mm3 in 30 days, and 298.97 mm3 in 40 days. The tumor even grew smaller in some cases, and the growth rate dropped significantly in general.
The findings of this study are not only applicable to anticancer drug-resistant cancers, but also to other refractory cancers that show the characteristics of cancer stem cells. This is because cell death can be avoided by controlling the concentration of calcium ions in the cytoplasm when the tumor microenvironment deteriorates.
“Through this study, we confirmed the effect of concomitant administration of existing anticancer drugs and the lead substance (Candidate 13) for the treatment of anticancer drug-resistant cancer,” said Dr. Cheong. He added, “We will continue the research on therapeutic agents for refractory cancer treatment.”
The results of this study are expected to open up great possibilities for cancer treatment in general and for the development of anticancer drugs for resistant cancers, for which effective treatments have not been found so far. The research team has applied for related patents at home and abroad based on this study and also licensed the related technology to VeraVerse Co. Ltd. in Korea and CKP Therapeutics, Inc. (Massachusetts Medical Device Development Center, Lowell MA 01852) based in Boston, USA for the development of anticancer drugs to push ahead with the derivation of additional lead compounds. Yonsei University Medical Center, with the research team playing a central role, is continuing its collaborative research with domestic and foreign corporations and is preparing for additional technology transfers and commercialization in the clinical field.
In recognition of the outstanding results of this research, the researchers were awarded Hanbitsa (People Who Brought Glory to Korea) by the Biological Research Information Center of Pohang University of Science and Technology (POSTECH).
Inquiry